ECG/EKG Cables, Leadwires, and Monitoring Equipment Guide
ECG and EKG equipment are now crucial for diagnosing and monitoring heart diseases. This thorough reference covers ECG and EKG cables, leadwires, monitoring equipment, interpretation, and testing.
ECG/EKG Basics
Modern medicine uses electrocardiography (ECG) and electrocardiograms (EKG) to assess heart electrical activity. These tests help diagnose and monitor heart diseases by revealing a patient's cardiovascular health. This page explains ECG and EKG's purpose, procedure, interpretation, and healthcare importance.
ECG/EKG Basics
Start with the fundamentals to understand ECG and EKG. ECG and EKG are interchangeable diagnostic terminology. Electrocardiograms measure heart electrical impulses non-invasively. Medical personnel use waveforms to evaluate cardiac rhythm, uncover irregularities, and diagnose illnesses. These impulses' waveforms help doctors diagnose heart diseases, cardiac rhythms, and anomalies.
ECG/EKG Functions: How?
Electrodes are attached to the patient's chest, arms, and legs for an ECG or EKG. These electrodes record heart electrical activity, which is graphed or shown. The ECG/EKG waveform shows the heart's depolarization and repolarization, revealing its function.
Healthcare's ECG/EKG Needs
Cardiology relies on ECG and EKG examinations in many clinical situations. ECG and EKG are crucial healthcare tools for these reasons:
ECG and EKG diagnose arrhythmias, myocardial infarctions, and conduction abnormalities.
Risk Assessment: These tests assess cardiovascular risk and identify people who may need additional therapies or prevention.
Treatment Monitoring: ECG and EKG help assess cardiac drugs, treatments, and procedures. They enable doctors to assess treatment responses and adapt.
Screening: Electrocardiography is used to test people with suspected cardiac disease or at risk due to medical problems or lifestyle.
Common Questions
ECG or EKG?
-
ECG and EKG are the same diagnostic exam.
Do ECGs hurt?
-
Electrodes on the skin make it painless. Non-invasive and painless.
ECG/EKG duration?
-
ECGs and EKGs take 5–10 minutes. The test time depends on patient condition and demand.
ECG or EKG for anyone?
-
ECG and EKG exams are generally safe. However, a doctor must assess if the test is necessary for your situation.
ECGs and EKGs detect what?
-
ECGs and EKGs can identify irregular heartbeats, heart muscle injury, conduction issues, and heart attacks.
ECG/EKG results: reliable?
-
ECG/EKG data are reliable but require expert interpretation. A skilled healthcare practitioner must assess the results for accurate diagnosis and treatment.
ECG Cables
Leadwires and cables connect the patient to the ECG machine during electrocardiography (ECG) and EKG testing. These components transmit electrical impulses from the body's surface to the equipment, enabling accurate heart electrical activity monitoring and analysis. ECG and EKG technicians must understand the importance of ECG leadwires and cables.
ECG Leadwire and Cable Function
ECG leadwires and cables send heart impulses to the ECG machine. Electrodes on the patient's body pick up these impulses, which the system sends through leadwires for processing and analysis. ECG and EKG results depend on leadwire and cable quality.
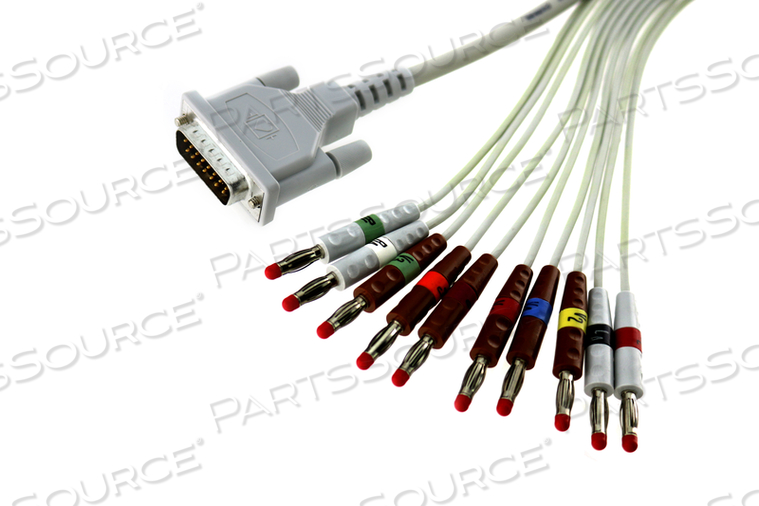
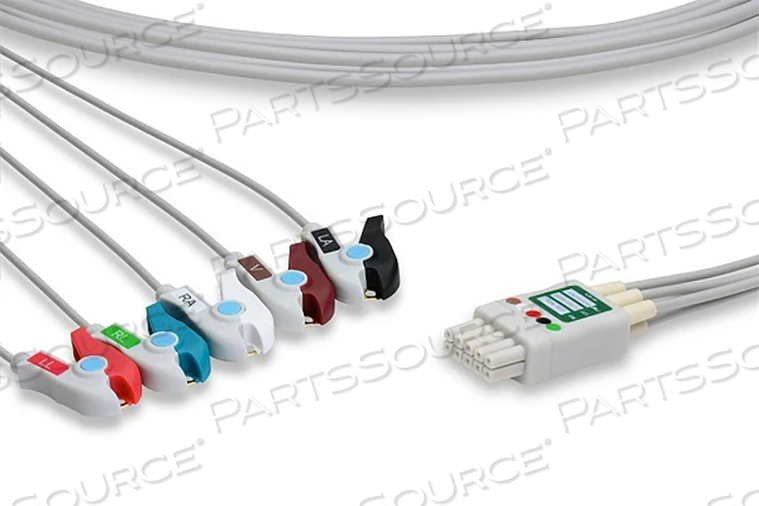
ECG Cables and Leadwires
Leadwires: Flexible cables link electrodes to ECG machines. They come in various lengths and configurations to suit patient positioning and demands. Leadwires are color-coded to guarantee proper electrode-machine connection.
Electrode Connectors: These connectors on the leadwires make electrode attachment easy and secure. Depending on the electrodes, electrode connectors are snap, clip, or banana plug.
Patient-end connections: These connections connect the leadwires to the electrodes on the patient's body. They are color-coded to match the electrodes for proper placement.
ECG Machine Connectors: These connectors accept patient-end connectors. They securely link leadwires to the machine to transfer electrical signals.
ECG Leadwire and Cable Types
Disposable Leadwires: These leadwires are used in hospitals for infection control. Disposable leadwires save time by eliminating patient cleansing and disinfection.
Reusable Leadwires: Durable materials make reusable leadwires last longer. To prolong their use, they can be cleaned, disinfected, and maintained.
Trunk cables connect leadwires to the ECG machine. These cables come in numerous lengths and combinations for therapeutic versatility.
ECG Leadwire and Cable Maintenance
ECG leadwires and cables must be properly maintained to last. Key considerations:
Check leadwires and cables for fraying, fractures, and loose connections. Replace damaged components immediately to avoid signal loss or erroneous readings.
To avoid patient cross-contamination, clean and disinfect reusable leadwires according to manufacturer recommendations.
Bending, twisting, or dragging leadwires and cables can damage connections and impede signal transmission.
Avoid dust, moisture, and extreme heat or cold when storing leadwires and cables.
ECG leadwires and cables allow the ECG machine to accurately detect and transmit electrical impulses from the patient's body. These components protect data and aid in diagnosis.
ECG leadwires and cables must be maintained for best performance and longevity. To avoid signal loss or erroneous measurements, check for fraying or loose connections. Damaged parts must be replaced immediately.
To avoid patient cross-contamination, clean and disinfect reusable leadwires according to manufacturer recommendations. Use leadwire and cable-safe cleaning products and methods.
Avoid bending, twisting, or pulling ECG leadwires and cables, since this might weaken the connections and cause signal interference or loss. Leadwires and cables must also be stored properly. To function, dust, dampness, and high temperatures should be avoided.
ECG and EKG technicians should learn about leadwires and cables. This allows clinical context and patient-needs-based selection. Reusable leadwires are durable and cost-effective, whereas disposable leadwires are convenient and infection-free.
Trunk cables, which connect leadwires to the ECG machine, exist in various lengths and designs for clinical versatility. Accurate signal transmission requires proper leadwire connections to electrodes and ECG machine interfaces.
ECG and EKG examinations require leadwires and cables. They help the ECG machine accurately identify and transmit electrical signals from the patient's body. ECG and EKG results depend on leadwire and cable upkeep and selection. Healthcare workers can maintain these vital diagnostic instruments by following instructions.
Interpreting ECG Axis
Healthcare practitioners must comprehend the ECG axis to interpret ECGs and EKGs. The ECG axis shows heart conduction direction. ECG axis interpretation reveals heart structure, rhythm, and anomalies. This article explains the ECG axis and clinical interpretation.
ECG Axis?
Heart electrical depolarization and repolarization follow the ECG axis. The ECG amplitude and direction determine it. The axis shows the average electrical flow during a cardiac cycle. the leader
ECG Axis Determination
Healthcare practitioners estimate the ECG axis by analyzing Lead I and Lead AVF electrical activity.
Lead I records right-left arm electrical activity. Lead I deflections of positive or negative imply leftward or rightward electrical flow, respectively.
Lead AVF: This lead monitors electrical activity between the left leg and the right arm (left arm average). Positive lead AVF deflection indicates downward flow, whereas negative deflection indicates upward flow.
Healthcare experts can estimate the ECG axis from Leads I and AVF deflections and evaluate if it is normal or abnormal.
ECG Axis
Normal ECG axis is -30 to +90 degrees. The axis is normal within this range. The axis is usually 0–90 degrees in healthy people.
ECG Deviations
ECG axis deviations may suggest heart problems or structural anomalies. ECG axis deviations include:
Left Axis Deviation (LAD): The axis is moved to the left beyond normal. Left ventricular hypertrophy, myocardial infarction, and conduction problems can cause it.
Right Axis Deviation (RAD): The axis is displaced right beyond normal. Chronic lung illness, right ventricular enlargement, and anatomical anomalies cause it.
Extreme Axis Deviation: An extreme axis deviates from the regular range (-90 to -30 degrees or +90 to +180 degrees). It appears in dextrocardia, ventricular septal abnormalities, and complicated congenital heart disorders.
Interpreting ECG Axis
ECG axis interpretation is clinically useful. It diagnoses, treats, and tracks heart problems. ECG axis abnormalities may require echocardiography or additional ECG leads to detect underlying diseases.
ECG/EKG analysts must understand the ECG axis and its interpretation. ECG axis can be determined from Leads I and AVF electrical activity, revealing cardiac architecture, rhythm, and anomalies. Deviations from the normal axis range can suggest certain cardiac diseases or structural abnormalities, prompting clinical decision-making and additional inquiry.
ECG and Cardiac Monitoring
Cardiovascular healthcare requires ECG testing and cardiac monitoring. These tests examine cardiac function, detect problems, and monitor heart patients. This page explains ECG testing, heart monitoring, and its clinical applications.
ECG Testing Overview
Electrocardiogram (ECG) testing measures heart electrical activity non-invasively. Electrodes on the patient's body record heart electrical impulses. Electrocardiograms reveal the heart's rhythm, pace, and function.
ECG Testing Goal
Cardiovascular ECG testing has many uses:
Diagnosis: ECG testing diagnoses arrhythmias, myocardial infarction (heart attack), conduction abnormalities, and structural abnormalities.
Risk Assessment: ECGs assess cardiovascular events like heart attacks and strokes. ECG abnormalities can suggest risk and guide further research or treatment.
ECG testing monitors cardiac drugs, treatments, and procedures. ECG waveform changes can reflect therapy response and help doctors adapt therapies.
Preoperative Evaluation: ECG testing assesses cardiac health and identifies underlying problems that may affect surgical outcomes.
ECG Tests
Clinical ECG tests include:
Resting ECG: Most common ECG test. The patient lies immobile as electrodes are put on specified chest, arm, and leg locations. The patient's resting ECG measures heart electrical activity.
Exercise Stress Test: The patient walks or pedals on a treadmill or exercise bike while the ECG is monitored. This test checks for coronary artery disease and exercise-induced arrhythmias by measuring the heart's response to activity.
Holter Monitoring: A portable ECG gadget called a Holter monitor captures the heart's electrical activity for 24–48 hours or more. This monitoring can detect intermittent arrhythmias and evaluate intermittent symptoms.
Event Monitoring: Event monitoring is like Holter monitoring but utilized for longer periods. When palpitations or dizziness occur, the patient's portable gadget records the ECG.
Cardiac Monitoring Overview
Cardiac monitoring measures and records the heart's electrical activity. ECG, telemetry, and implanted cardiac monitors can be used.
Cardiac Monitoring Goal
Cardiac monitoring has many uses.
Continuous cardiac monitoring can reveal arrhythmias that an ECG test may miss. This is crucial for individuals with suspected arrhythmias, sudden cardiac death risk, or antiarrhythmic medication.
Event Recording: Cardiac monitoring records cardiac events and symptoms. This helps identify the rhythm or arrhythmia causing palpitations, chest discomfort, or dizziness during episodes.
Long-Term Monitoring: Cardiac monitoring provides a prolonged picture of the heart's electrical function. For patients with chronic or recurrent cardiac problems, this allows doctors to track trends, evaluate treatment efficacy, and alter medications.
Risk Stratification: Cardiac monitoring helps patients with cardiovascular diseases or high cardiac risk stratify their risk. Healthcare providers can uncover high-risk patterns or abnormalities by continuously monitoring the heart's electrical activity.
Heart Monitors
ECG Monitors: These portable gadgets can record the heart's electrical activity continuously or sporadically. Hospitals and cardiac events employ ECG monitoring.
Telemetry Systems: Wireless telemetry systems send patient ECG data to a central monitoring station. This lets doctors monitor several patients and retrieve vital cardiac data.
Implantable Cardiac Monitors (ICMs): Small devices implanted under the skin monitor the heart's electrical activity for months or years. In patients with unexplained syncope, palpitations, or recurring arrhythmias, these devices are employed for long-term monitoring.
Cardiovascular care includes ECG testing and monitoring. ECG testing supports diagnosis, risk assessment, and therapy effectiveness. Resting ECGs, exercise stress tests, Holter monitoring, and event monitoring serve diverse purposes depending on patient demands and clinical indications.
ECG monitors, telemetry systems, and implanted devices detect heart electrical activity continuously or intermittently. It detects arrhythmias, records symptoms, monitors patients over time, and stratifies risk.
ECG testing and cardiac monitoring help diagnose, treat, and monitor heart problems. Healthcare providers can enhance cardiovascular care by precisely analyzing the heart's electrical function.
ECG/EKG equipment helps diagnose and monitor heart disorders. The healthcare provider or patient decides on equipment, leadwires, and cables. ECG interpretation and testing are crucial for heart disease diagnosis and treatment.


